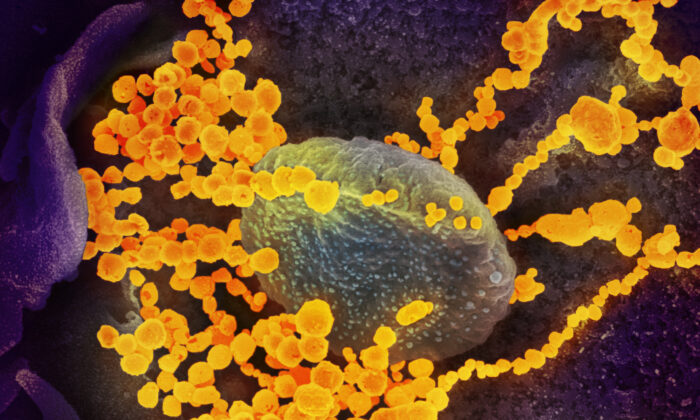
Fibrin binds to proteins from the SARS-CoV-2 virus to form blood clots that are difficult to break down, the authors found. This clotting then drives the various inflammatory and neurological symptoms seen in COVID-19 and long COVID, the researchers found. Previous studies have theorized that blood clotting is a consequence of inflammation.
However, the new Nature study, published on Wednesday, shows the reverse: that the clotting comes first. “Our study is the first to report causality for fibrin as the root of inflammation and brain pathology after COVID infection,” Katerina Akassoglou, senior author and professor of neurology at UCSF, told The Epoch Times on email. By blocking fibrin using a novel antibody, the researchers were able to reduce clotting and neurological symptoms, offering a new potential therapeutic for patients.

“We showed that the binding of fibrin to spike forms clots that have very high inflammatory activity,” Akassoglou said. Researchers tested their findings in mice, infecting them with COVID-19 Beta and Delta variants. They found fibrin bound to COVID-19 spike proteins to form irregular amyloid-like clots that are difficult to break down using traditional therapies.
The researchers found that the spike and fibrin clots would be deposited in the blood vessels, lungs, and the brains of mice, leading to scarring and inflammation, potentially driving breathing and neurological problems seen in long COVID-19 patients. In the brain, COVID-19 infection caused protein deposits to be formed in the mice brains, triggering inflammation in brain cells. “Furthermore, we showed that fibrin induces toxic inflammation, while suppressing NK cells that clear the virus,” Akassoglou said.
Mice that were genetically modified to not produce the right fibrin proteins had less inflammation when infected with COVID-19, the authors found. Their cancer-fighting natural killer cells were also more active at clearing out COVID-19 spike proteins. Researchers exposed mice to subunits of the spike protein rather than the complete virus and clots still formed.
They suggest that in long COVID, it may be the remnant spike proteins driving the disease. While COVID-19 mRNA and adenovirus vaccines cause the body to produce spike proteins, the authors said that the vaccines would not cause these clots. “In general, COVID-19 RNA vaccines lead to small amounts of spike protein accumulating locally [.
..] and the protein is eliminated,” they wrote.
The study, which was funded by the U.S. Centers for Disease Control and Prevention (CDC), found COVID-19 vaccines were linked to few adverse events.
Though at certain doses, people who took the COVID-19 mRNA and/or adenovirus vaccines had a slightly increased odds of contracting various clotting diseases. Other clinicians, including Dr. Keith Berkowitz of Centers for Balanced Health and nurse practitioner Scott Marsland at the Leading Edge Clinic, disagreed with the UCSF researchers’ statements in the study.
Marsland and Dr. Paul Marik, chairperson of Front Line COVID-19 Critical Care Alliance, said that clotting is a common adverse reaction some people may experience following COVID-19 vaccination, though few studies have evaluated patients for such conditions. Mice that were previously infected with COVID-19 had an improvement in their inflammation, scarring, clotting, brain damage, and overall survival after being given the antibody.
Giving the antibody for prevention similarly reduced inflammation and organ damage. Common anticoagulants, which are medications that prevent blood clots, can increase bleeding risks while this antibody does not increase the risk of bleeding, the authors said. It is highly selective for the inflammatory form of fibrin and does not have the adverse effects like those observed with some anticoagulants, Akassoglou said.
A humanized version of Akassoglou’s fibrin-targeting immunotherapy is already in Phase 1 safety and tolerability clinical trials in healthy people funded by the biotechnology company Therini Bio. Marsland said he found sulodexide, a drug not FDA-approved in the United States but approved in Europe, to be highly effective in treating clotting without increasing people’s risks of bleeding. Sulodexide is a drug that is used to treat thrombotic diseases and diabetic neuropathy.
.