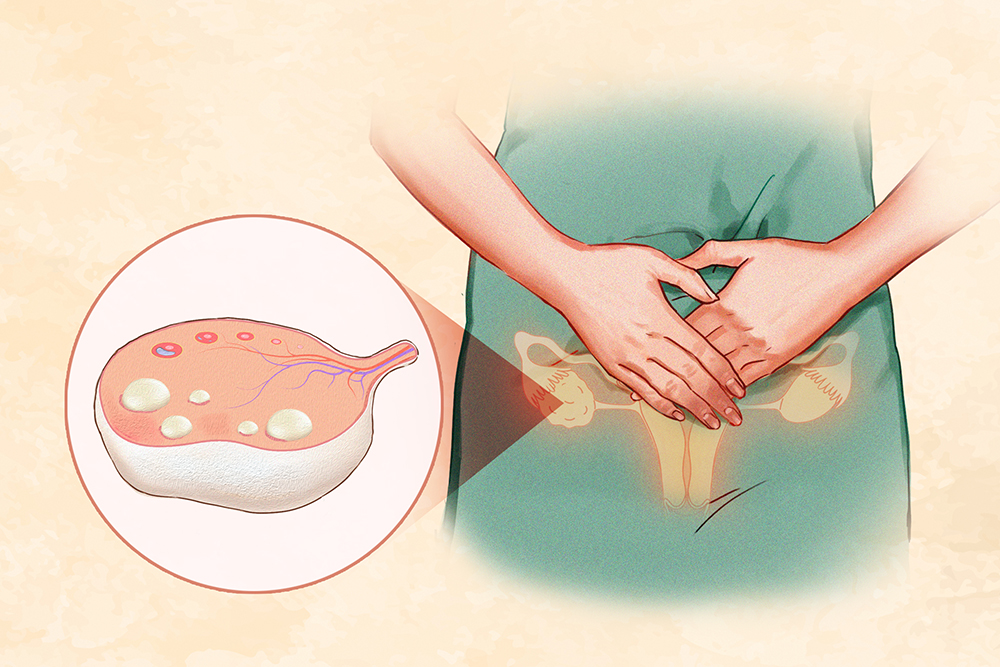
Polycystic ovary syndrome (PCOS) is a condition of hormonal imbalance affecting women and girls of reproductive age. It can cause menstrual cycle changes, increased facial and body hair, acne, ovarian cysts, infertility, and metabolic issues. Phenotype A: All three diagnostic criteria sets are present.
Phenotype B: Hyperandrogenism and ovulatory dysfunction are present. Phenotype C: Hyperandrogenism and polycystic ovarian morphology are present. Phenotype D: Ovulatory dysfunction and polycystic ovarian morphology are present.

Insulin-resistant PCOS: Women with PCOS frequently experience insulin resistance, where their bodies produce insulin but cannot use it effectively. This condition raises the risk of Type 2 diabetes. Inflammatory PCOS: PCOS is linked to chronic inflammation , which can disrupt ovulation and hormone production.
Research shows that PCOS patients often have higher levels of inflammatory markers. This inflammation is exacerbated by obesity and high insulin levels, with studies highlighting the interrelated effects of hyperinsulinemia, obesity, hyperandrogenism, and inflammation. Adrenal PCOS: A subgroup of women with PCOS may have elevated levels of adrenal hormones than average.
Hidden-cause PCOS: People use this term to describe PCOS cases where the typical symptoms and signs of the condition are present, but the underlying cause or contributing factors are not immediately apparent. The Essential Guide to Breast Cancer: Symptoms, Causes, Treatments, and Natural Approaches Yeast Infection: Symptoms, Causes, Treatments, and Natural Approaches Absent or irregular menstruation: PCOS can cause high levels of androgens and insulin, disrupting the menstrual cycle. This may result in heavy, light, irregular, or absent periods, and some girls may not start menstruating at all.
Irregular or absent ovulation: Irregular ovulation can lead to infertility. Bleeding without ovulation, known as an anovulatory period, can also take place. Infertility or reduced fertility: While PCOS is a leading cause of infertility, many women with the condition can still become pregnant, but they face a higher risk of complications.
Hirsutism (excess hair growth): Due to increased androgen levels, PCOS can lead to the development of excess hair, which is typically thicker and darker than usual and often appears in areas where men commonly grow hair, such as the chin, upper lip, and around the nipples. About 60 percent of women with PCOS experience this symptom. Despite having similar androgen levels, women of Eastern European descent are more likely to exhibit hirsutism, while Asian women tend to have little or no excess hair growth.
Acne or s eborrhea (excessive oily skin) : In PCOS, increased androgen levels can enlarge oil glands in the skin, leading to acne breakouts. As a result, young women with PCOS may experience persistent and severe acne. Acanthosis nigricans (dark skin patches): In areas such as the armpits or neck, rough, dark, and soft patches of skin may appear.
Anxiety and depression: PCOS can make women feel stressed out, anxious, and depressed. Additionally, other symptoms of PCOS (e.g.
, infertility or hirsutism) may lead to these feelings. Weight issues: Women with PCOS may face a higher risk of unhealthy weight. Managing weight can be challenging due to hormonal imbalances affecting appetite and regulating hunger.
Obesity affects up to 50 percent of PCOS patients. However, some patients are underweight , though this is rare. Cystic or enlarged ovaries: Cystic ovaries contain multiple tiny fluid-filled sacs, or cysts.
Hyperlipidemia (high blood fats): Hyperlipidemia is characterized by increased triglycerides, total cholesterol, and low-density lipoprotein (LDL) cholesterol (“bad” cholesterol), along with decreased high-density lipoprotein (HDL) cholesterol (“good” cholesterol). Sleep problems: One example is sleep apnea. High blood pressure.
Pelvic pain. Skin tags. Alopecia (hair loss).
Fatigue. Low energy. Headaches.
Mood swings. 1. Genetics 2.
Hormone Imbalance Testosterone: Although testosterone is the primary male hormone, it is also produced in small amounts by women. Women with PCOS may produce more testosterone than usual, leading to symptoms such as excess hair growth, acne, and irregular periods. Luteinizing hormone: Luteinizing hormone helps trigger ovulation.
However, in women with PCOS, high levels of this hormone can affect the ovaries abnormally, contributing to the production of more male hormones and further disrupting the menstrual cycle. Sex hormone-binding globulin (SHBG): SHBG is a protein that binds to testosterone in the blood while reducing its effects. If SHBG levels are low, there will be more unbound testosterone, exacerbating PCOS symptoms.
Estrogen: Women with PCOS may have lower estrogen levels. Family history of PCOS. Infections: Infectious mediators can contribute to PCOS.
Toxin exposure: In animal studies , endocrine-disrupting chemicals , such as those found in synthetic fragrances and the industrial plasticizer bisphenol A (BPA), have been shown to induce androgen production and insulin resistance . Women with PCOS tend to accumulate more BPA in their bodies, which could lead to an increase in symptom severity. Obesity or metabolic disorders.
Early puberty. Age: Women in their 20s and 30s are more at risk due to being in their prime reproductive years. Race: The prevalence among patients aged 16 to 40 was 5.
2 percent across all racial and ethnic groups. Incidence rates were as follows: 6.8 percent for Hispanics, 5.
2 percent for whites, 4 percent for Asians, 6.9 percent for Native Americans, 4.6 percent for African Americans, and 7.
6 percent for Hawaiians and Pacific Islanders. Therefore, Native Americans and Hawaiian/Pacific Islanders face an increased risk. Oligo- or anovulation: Infrequent or absent ovulation (amenorrhea).
Ovulatory dysfunction like this occurs when a woman has irregular or fewer than nine periods per year or does not ovulate. Hyperandrogenism: Hyperandrogenism refers to the presence of excessive levels of male sex hormones, such as testosterone. Clinical signs include excessive hair growth, acne, or male pattern baldness.
Polycystic ovaries: Each ovary cyst represents a follicle holding an egg. Twelve or more follicles in at least one ovary measuring 2 to 9 millimeters in diameter or increased ovarian volume (>10 cm3). Tests Estrogen level.
Follicle-stimulating hormone (FSH) level. Luteinizing hormone level. Testosterone level.
Progesterone level. Fasting glucose (blood sugar) and other tests for insulin resistance. Lipid level.
Pregnancy test (human chorionic gonadotropin test): A pregnancy test is performed in diagnosing PCOS primarily to rule out pregnancy as a cause of symptoms such as missed periods or irregular menstrual cycles since these symptoms are common in both pregnancy and PCOS. Prolactin level: Although the causality of the association between increased prolactin levels and PCOS remains unclear, higher prolactin levels could inhibit ovulation and result in polycystic ovarian morphology. Thyroid function tests.
Prediabetes: Up to 35 percent of women with PCOS develop prediabetes, characterized by elevated blood glucose levels that are higher than normal but not yet high enough to be classified as diabetes. Type 2 diabetes: By age 40, approximately 10 percent of overweight women with PCOS develop abnormally high blood glucose levels. Subfertility or infertility: Up to 70 percent of women with PCOS experience fertility issues.
High blood pressure. Cardiovascular problems: In the long run, excess male hormones increase the risk of cardiovascular disorders. Uterine cancer: Uterine cancer is the most prevalent cancer of the female reproductive system, originating as a malignant tumor in the cells of the uterus.
Its two types include the common endometrial cancer and rare uterine sarcoma. PCOS may lead to uterine cancer due to irregular and infrequent menstruation, along with increased estrogen levels. Gestational diabetes: Blood sugar levels rise during pregnancy.
High LDL cholesterol. Sleep apnea. Stroke.
Obesity-related complications. Metabolic syndrome: Increased male hormones can also cause metabolic syndrome and contribute to obesity. Depression and anxiety: Women with PCOS also have higher rates of major depression, recurrent depression, anxiety, and suicide attempts.
Nonalcoholic fatty liver disease (NAFLD): Women with PCOS have a higher risk of developing NAFLD. Sexual health problems. Endometrial hyperplasia: Endometrial hyperplasia, the thickening of the uterine lining, is a particular concern for women with PCOS who are obese, diabetic or prediabetic, insulin resistant, or have a long history of menstrual irregularities.
This condition is relatively uncommon. Treatment for PCOS varies based on factors such as age, symptom severity, overall health, and whether future pregnancy is desired. Change in diet and activity: A healthy diet and increased physical activity can aid in weight loss, alleviate PCOS symptoms, improve insulin efficiency, lower blood glucose levels, and potentially enhance ovulation.
Medication to cause ovulation: These medications carry risks, including an increased risk of multiple births (such as twins) and ovarian hyperstimulation, which can lead to symptoms such as abdominal bloating and pelvic pain. Miscarriage High blood pressure Gestational diabetes Potentially fatal preeclampsia Birth control pills: These treat hormonal imbalances and regulate menstruation. They can also help reduce abnormal hair growth and acne when taken for several months.
Diabetes medication: These can reduce insulin resistance in PCOS. Other medications: Women with PCOS often require several medications to manage symptoms such as hirsutism, anovulation, and menstrual irregularities. One example is androgen-blocking medication.
1. Dietary and Physical Therapies Exercise and calorie-restrictive diets are the best first-line interventions for weight loss in overweight and obese PCOS women and adolescents. Exercise can help reduce insulin resistance, body weight, and glucose levels, but equally significantly, it also boosts self-esteem.
2. Menstrual Abnormality Treatments Hormonal contraceptives: The first-line treatment for menstrual abnormalities, hirsutism, and acne is hormonal contraceptives, either oral, patches, vaginal rings, or hormone-releasing intrauterine devices (IUDs). All of these may decrease luteinizing hormone levels, indirectly decreasing ovarian androgen production and increasing SHBG, and stop the abnormal growth of the uterine lining.
Therefore, they are highly effective for symptoms of hyperandrogenism and controlling the menstrual cycle. Metformin: Metformin, a diabetes medication, is also used as a second-line treatment for menstrual irregularities in patients who cannot use hormonal contraceptives. It helps restore regular menstrual cycles, assists in weight loss, and reduces insulin resistance, particularly benefiting adolescents and obese patients.
The Endocrine Society recommends starting metformin for PCOS patients with Type 2 diabetes or impaired glucose tolerance who do not respond to lifestyle changes. Additionally, it can improve waist-to-hip ratio, menstrual regularity, and vascular markers in nonobese women with PCOS. 3.
Infertility Treatment Another treatment option is clomiphene citrate, a selective estrogen receptor modulator (SERM) and competitive inhibitor of estrogen receptors (ERs) with mixed agonist and antagonist activity. It aids the hypothalamus by binding to estrogen receptors for an extended period, depleting them and blocking the negative feedback effect of circulating estrogen. 1.
Medicinal Herbs Chasteberry (Vitex agnus-castus): The chasteberry plant , also known as the chaste tree, is native to the Mediterranean region and Asia. Its fruit contains natural chemicals called monoterpenoids , such as alpha-pinene. It also includes other compounds that help lower prolactin levels.
These mechanisms can help prevent cyst formation in the ovaries and may be beneficial for treating PCOS. Turmeric (Curcuma longa): Turmeric is derived from the root of the turmeric plant and has been used for centuries in Ayurvedic and Chinese medicine. Turmeric contains over 250 phytoconstituents, carbohydrates, proteins, terpenes, and resins.
Among them, curcuminoids, which comprise a small percentage of the resins, are the main secondary metabolites. These curcuminoids can effectively treat PCOS, as they help reduce the follicular sheath, enhance the menstrual cycle, and improve ovulation. Consequently, turmeric may improve the histological features of polycystic ovaries.
Flax (Linum usitatissimum): Flaxseed is high in lignans and has been demonstrated to lower androgen levels in men with prostate cancer. In a 2020 study , 41 PCOS patients were randomly assigned to either receive 30 grams of flaxseed powder daily along with lifestyle modifications or to follow only lifestyle modifications for 12 weeks. As it turned out, the treatment of the first group was more effective than that of the second group, as flaxseed supplementation led to a significant decrease in body weight, waist circumference, and body mass index (BMI) among women with PCOS.
2. Diet Mediterranean diet: The Mediterranean diet, which excludes saturated fats, processed meats, and refined sugars, is an effective way to combat inflammation. With its focus on nonstarchy vegetables, fruits, lean proteins, healthy carbs, and low-fat dairy, this diet can also help women with PCOS improve their health and prevent complications.
Ketogenic diet: The ketogenic diet is a high-fat, low-carbohydrate eating plan. A 2023 study found that a short-term keto diet (for at least 45 days) may help improve hormonal imbalances commonly associated with PCOS. Omega-3 rich fish Olive oil Legumes and beans Nonstarchy vegetables, including leafy greens, tomatoes, mushrooms, peppers, broccoli, cauliflower, snow peas, celery, and fennel Whole grains Whole fruits, which have a high fiber content to help with satiety and digestion and slow sugar absorption Fried foods Red and processed meats Processed snacks Sugary cereal Sugary beverages, including sodas, sweetened teas, and sports drinks Alcohol Refined flour products 3.
Supplements Inositol: Inositol is a type of sugar‐alcohol found in fruits, beans, grains, and nuts. A 2023 systematic review of 26 studies involving 1,691 PCOS patients found inositol an effective alternative to metformin for treating the condition. Another 2022 meta-analysis showed that oral inositol supplementation might reduce BMI and could be considered an adjunct treatment for improving BMI.
Berberine: Berberine is a compound in various plant species, often used in traditional Chinese medicine (TCM) and the Ayurveda medical system. It may help manage PCOS by addressing multiple aspects of the condition with fewer side effects than pharmaceuticals. As per a 2021 review , it can improve insulin resistance , lower serum androgen levels, regulate lipid metabolism, and reduce chronic inflammation in PCOS patients.
Berberine is often combined with metformin, cyproterone, and other medications to enhance therapeutic outcomes for PCOS. Chromium: Chromium is an essential trace metal. In a 2017 meta-analysis , chromium supplementation was found to lower serum insulin and free testosterone levels while improving body weight in PCOS patients.
In a 2018 study examining the effects of eight weeks of chromium supplementation in infertile women with PCOS who were preparing for in vitro fertilization (IVF), chromium was found to improve their glycemic control, reduce some cardiometabolic risk factors, and lower oxidative stress. Seed cycling: Seed cycling means eating different seeds during the two phases of the menstrual cycle. A 2023 article showed that seed cycling effectively improves hormonal disturbances in women with PCOS.
Additionally, a 2021 study indicated that omega-3 fatty acids from flaxseeds, pumpkin, sesame, and sunflower seeds could be a novel treatment for PCOS. 4. Acupuncture 5.
Electro-Acupuncture 6. Yoga 7. Mindfulness-Based Stress Reduction 8.
Tai Chi Avoiding smoking and excessive drinking Maintaining a healthy weight Eating a balanced diet composed of fruits, vegetables, whole grains, lean meats, fish, and chicken while reducing sugar, salt, and caffeine intake Eating regular meals (for instance, not skipping breakfast) Exercising regularly, getting at least 150 minutes of exercise a week.